|
 |
- Search
| Arch Aesthetic Plast Surg > Volume 30(1); 2024 > Article |
|
Abstract
Asians typically exhibit prominent zygomas; therefore, several attempts have been made to reduce these structures to achieve a softer appearance. The intraoral approach is preferred because of its shorter surgical duration and lower invasiveness; however, it is associated with serious complications, such as nonunion. In revisional surgery, the intraoral approach poses limitations in accessing the upper part of the zygoma and the lateral orbital rim area due to its restricted operative field. Therefore, we developed an intraoral interpositional bone graft technique that enabled almost complete reconstruction. A 40-year-old woman presented with persistent depression in the left infraorbital and cheek regions after two revision operations after reduction malarplasty. Based on computed tomography (CT) scan findings, reconstruction using bone grafts was planned. Calvarial bone was harvested and divided into cortical and cancellous parts. The cortical bone was sculpted into an L-shape and inserted into the gap between the maxilla and the lower zygoma body. The hard-to-reach lateral orbital rim area was filled with cancellous bone without fixation. Follow-up CT scans showed that the cortical bone grafts were well-maintained and stabilized with titanium plates, while the cancellous bone had undergone significant resorption and was replaced by new bone, indicative of successful natural healing.
Asians generally tend to have more prominent zygomas than Westerners. Many Asians seek to reduce the size of their zygomas to achieve a softer facial appearance. Among the various methods of malar reduction, the intraoral approach is preferred due to its minimally invasive nature and shorter surgical duration [1]. However, this approach offers a limited surgical field of view for achieving three-dimensional fixation after malar reduction. Additionally, the external forces exerted by the masseter muscle can lead to nonunion, which may result in complications such as facial depression and asymmetry. Furthermore, prolonged nonunion can cause continuous bone resorption at the exposed bone surface, preventing bone-to-bone contact and leading to a gap even after malar repositioning [2]. Research on the treatment of nonunion with bone resorption is limited. Some studies have introduced a camouflage technique that involves onlay grafting of rib bone onto the bone gap [3]. However, the gap is often a three-dimensional space, and onlay grafts alone may not be adequate to correct the entire bone gap, especially in the lateral orbital rim area. We propose a method that utilizes an interpositional bone graft from both the cortical and cancellous parts of the calvarial bone to achieve correct three-dimensional nonunion to achieve correct three-dimensional union.
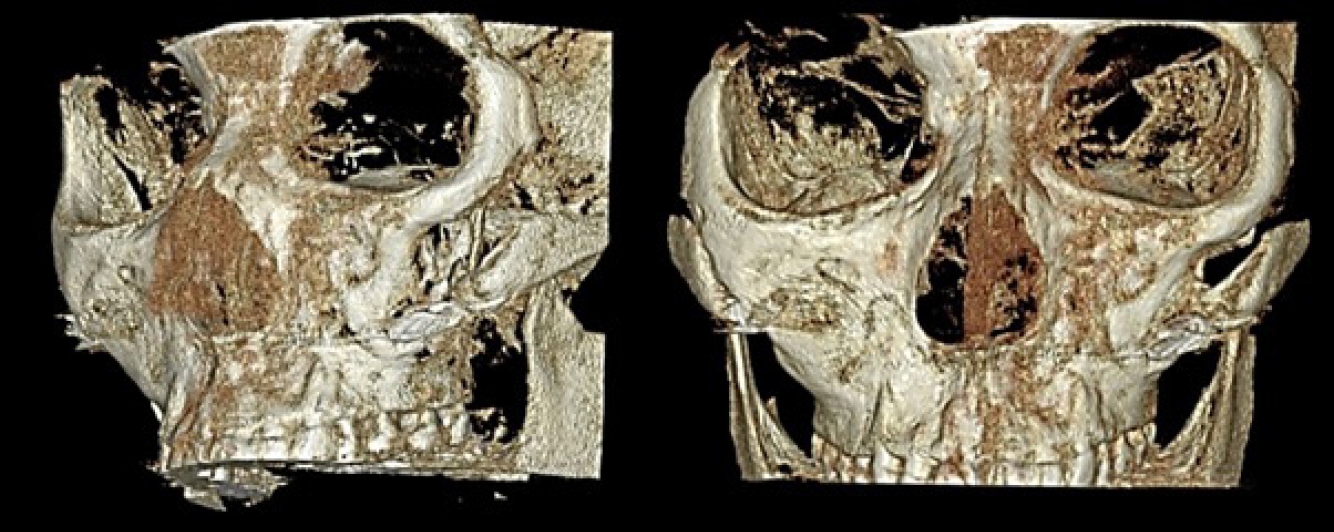
A 40-year-old patient presented to Inje University Busan Paik Hospital with persistent depression in the left infraorbital and cheek regions, which persisted after two revision operations performed 3 years prior, following a reduction malarplasty. The patient had initially undergone reduction malarplasty through an intraoral approach, with a single titanium plate used for fixation. Unfortunately, the titanium fixation proved inadequate during the first surgery, resulting in asymmetry and bone gaps due to excessive bone removal. Six months later, she experienced mild cheek drooping and an oblique depression at the inferolateral side of the lateral orbital rim. A subsequent revision malarplasty using Goretex failed to correct the asymmetry and depression. Clinical examination revealed no functional impairments, such as limited mouth opening or pain, nor any signs of infection. Preoperative facial photographs (frontal, oblique, and worm’s-eye views) were taken to document and compare the results. Nonunion from the previous operations was confirmed using three-dimensional computed tomography (CT) scans (Fig. 1). The CT images showed that the malar complex was dislocated inferiorly and externally rotated, creating a bone gap that extended from the frontonasal wall to the external orbital rim. The bone surface around the gap appeared irregular due to resorption. Based on these CT findings, we decided to reconstruct the nonunion using bone grafts. Surgery was performed under general anesthesia. A solution of 0.5% lidocaine with epinephrine (1:100,000) was injected into the vestibular labiobuccal groove. We reopened the tissue intraorally along the pre-existing incision line. Upon exposing the anterolateral aspect of the zygomaticomaxillary complex, the previously implanted Goretex was completely removed. We identified an extensive large bone gap resulting from an inadequate malarplasty and noted that a portion of the lateral orbital rim was absent (Fig. 2). The margin was debrided, with resorbed bone and surrounding connective tissue being removed. An incision was made anterior to the ear, the malunion was addressed and stabilized, and the maxillary bone gap was assessed and measured.
Calvarial bone grafts were harvested from the parietal region to reconstruct the infraorbital bone defect. An incision was made above the termination of the temporal muscle, and a full-thickness scalp flap was elevated. The bone grafts were shaped to a predetermined size. To facilitate removal, a beveled edge was created around the calvarial outer table graft using a bone scraper (SafeScraper Twist; META), followed by the use of a reciprocating saw. Substantial quantities of cortical and cancellous bone were harvested with the scraper.
The harvested bone grafts were separated into cortical and cancellous components. During reconstruction, the cortical bone was fashioned into an L-shape and positioned in the space between the maxilla and the lower zygomatic body (Fig. 3). The junction between the graft and bone was firmly secured with 5-hole mini plates and screws. The cortical bone served to fill most of the bone defect, while the cancellous bone was used to fill the remaining regions, specifically the lateral infraorbital rim and the upper zygomatic bone.
To minimize muscle movement, the patient was advised to follow a soft mixed diet for 4 weeks postoperatively, and care was taken to avoid fully opening the mouth. The patient returned to the hospital for follow-up evaluations, which included facial photography and CT scans at 5 months and 2 years post-surgery. The comparative results from before the surgery, at 5 months postoperatively, and at 2 years postoperatively demonstrated the correction of the depression around the left zygomatic area (Fig. 4). The images also revealed that the depression around the left cheekbone had been corrected and that the contour appeared smooth following the reconstruction with the interpositional graft (Fig. 5). The patient was satisfied with the outcome and did not require any further treatment.
There are two primary methods for malar reduction: coronal incisions and the intraoral approach. Coronal incisions provide a broader surgical field than the intraoral approach, which facilitates precise repositioning and fixation of the malar complex [4]. Furthermore, direct visual inspection of the frontozygomatic sutures enables proper fixation [4]. However, coronal incisions are less commonly used due to longer surgical times and a higher risk of complications, such as excessive bleeding, temporal paresthesia, and facial hollowing. As a result, many patients opt for the intraoral approach, despite its challenges, which include difficult osteotomy and fixation owing to limited surgical visibility [5]. Moreover, the rotational force exerted by the masseter muscle primarily affects the superior portion of the malar complex, causing displacement of the zygoma and downward pull on its body. This interference with the bony union can lead to bone resorption. Consequently, complications such as facial deformity, cheek drooping, or restricted jaw movement may occur, often necessitating reoperation [6].
Nonunion of the malar bone following reduction malarplasty is a significant complication that presents considerable challenges for correction [3]. Revision surgery aims to address the anatomical and functional issues resulting from nonunion. In instances where bone resorption has occurred due to nonunion, it is necessary to re-establish proper bone contact [4]. The connective tissue between the non-united bones should be removed, and a clean bone surface should be created through beveled osteotomy [2,4]. It is equally important to accurately reposition the malar complex and ensure its stable fixation. While osteotomy and repositioning may initially suffice, bone grafting becomes necessary after 4 months due to ongoing resorption and bone remodeling.
The choice of approach for revision surgery depends on the accessibility and ease of reconstruction of the resected areas during the initial surgery. A coronal incision is a definitive method for reconstructing large bone gaps that may result from inadequate malarplasty, as it allows precise reconfiguration and rigid fixation [4]. However, when using an intraoral approach, fixation in the lateral infraorbital region tends to be insufficient, which can lead to a depression in the lateral orbital area [3,7]. In some cases, fat grafts or fillers are employed alongside bone grafts, but these are incomplete solutions.
However, the authors achieved favorable outcomes using the intraoral approach with both cortical and cancellous calvarial bones. This success can be attributed to the functional matrix theory, as proposed by Moss and Rankow [8], which suggests that the growth of the craniofacial skeleton is influenced by signals from the surrounding soft tissues. According to this theory, the functional requirements of these tissues can initiate intracellular signaling that transforms biomechanical forces into bone formation [8]. Consequently, bone remodeling achieves a configuration that optimally resists mechanical stress [9]. Two years postoperatively, CT images of the patient revealed well-maintained cortical bone structures secured by titanium plates, alongside significant resorption of the cancellous bone, which was replaced by new bone, indicative of natural healing.
Various alloplastic bone graft materials, including calcium sulfate, calcium phosphate, tricalcium phosphate, and coralline hydroxyapatite, are options for midfacial reconstruction [10]. However, these materials can provoke host reactions, lead to migration, and cause implant displacement, which may result in asymmetrical outcomes [2]. Additionally, if atrophy occurs in the overlying soft tissue, the implant becomes more visible. Considering that the malar complex is frequently exposed to external impacts on the face, it is advisable to avoid the use of artificial materials to ensure the safety of the orbital rim [2].
Autogenous bone grafting is regarded as the gold standard for skeletal reconstruction of the midface [11]. Cancellous bone grafts have superior osteoconduction, osteoinduction, and osteogenesis properties, serving as scaffolds for bone regeneration and ensuring gradual ossification as the bone gap is filled [2,12]. Furthermore, cortical bone inserted as an onlay graft provides a bone bridge for bone formation and osteoconduction, offering support against soft tissue collapse and achieving greater bone volume [13,14]. Therefore, using cortical and cancellous calvarial bone enables a stable intraoral interpositional bone graft.
However, our approach has some limitations. We used calvarial bone as the donor site for the graft. Ideally, if an incision is required in the scalp area, it would be more efficient to perform both the surgical approach and the bone graft harvest through a single coronal incision, which provides a wider surgical field. Initially, we discussed the possibility of a coronal incision; however, due to the patient’s concerns about potential scarring on the scalp, we opted for minimal incisions to harvest the bone. Although using rib, pelvic, or iliac bones for bone grafting can prevent scalp scars, clinical experience has shown that grafts from calvarial bone have better volume retention, higher resistance to infection, and faster vascularization than those harvested from other sites [12,15]. Calvarial bone offers a substantial amount of cortical bone, and its diploic space is rich in cancellous bone, which is advantageous for bone grafting. Furthermore, the morbidity and complication rates associated with calvarial bone donor sites are low. The thickness and shape of the calvarial bone make it particularly well-suited for facial bone restoration, rendering calvarial bone grafts the preferred choice for facial reconstruction [15].
In conclusion, inadequate fixation after reduction malarplasty via the intraoral approach can lead to bone gaps due to the rotational forces exerted by the masseter muscle, particularly in the upper and lateral infraorbital regions of the zygoma. Coronal incisions are commonly employed when significant gaps are present in this area. However, our findings indicate that using an interpositional bone graft technique, which utilizes both cancellous and cortical parts of the calvarial bone, can facilitate near-complete reconstruction. This method involves leaving the posterior space without fixation and securing the anterior portion with cortical bone. Over time, the inserted bone graft remodels in response to the functional demands of the surrounding soft tissue, resulting in a natural-looking outcome. Two years postoperatively, CT scans showed that the cortical bone parts, stabilized by titanium plates, were well-preserved, and there was considerable resorption of the cancellous bone. This resorption was accompanied by the formation of new bone, signifying a natural healing process.
Notes
Ethical approval
This report was approved by the Institutional Review Board of Inje University Busan Paik Hospital (IRB No. 2023-08-027).
Patient consent
The patient provided written informed consent for the publication and use of her images.
Fig. 2.
(A) Intraoperative photography exposing the anterolateral aspect of the zygomaticomaxillary complex. (B) The Goretex from the previous surgery has been fully removed.
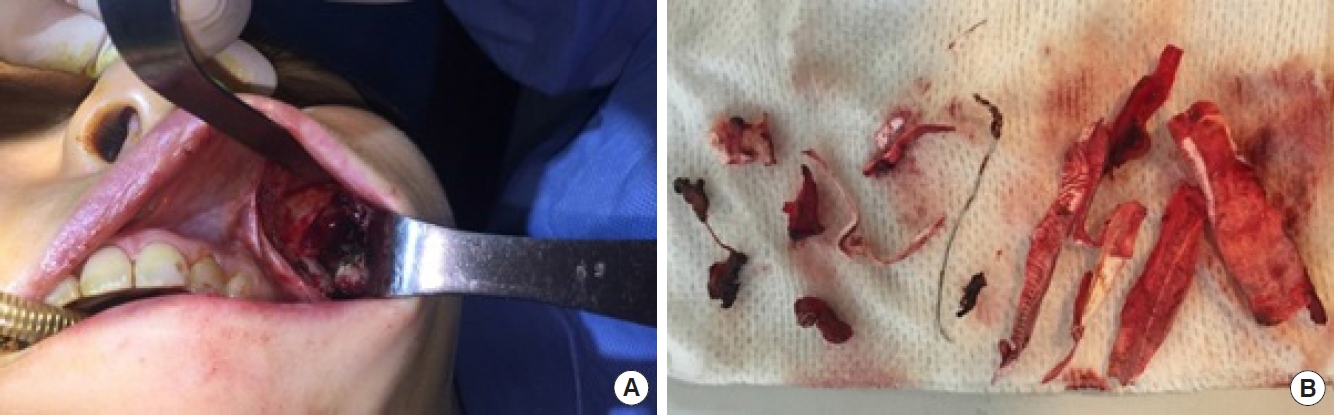
Fig. 3.
(A) Harvested calvarial bone. (B) Cortical bone has been trimmed into an L-shape to fit the maxilla and lower zygomatic body gap.

Fig. 5.
Patient photographs. (A) Preoperative patient photographs: the left cheekbone appears depressed and asymmetric because of malar nonunion and bone absorption. (B) Postoperative patient photographs at 2 years. The depression around the left cheekbones is corrected after reconstruction with an interpositional graft. The patient was satisfied, and there was no further requirement for treatment.

REFERENCES
2. Yoon SH, Jeong E, Chung JH. Malar relocation with reverse-l osteotomy and autogenous bone graft. Arch Craniofac Surg 2017;18:264-8.




4. Baek RM, Kim J, Lee SW. Revision reduction malarplasty with coronal approach. J Plast Reconstr Aesthet Surg 2010;63:2018-24.


5. Shetty SK, Saikrishna D, Kumaran S. A study on coronal incision for treating zygomatic complex fractures. J Maxillofac Oral Surg 2009;8:160-3.




6. Myung Y, Kwon H, Lee SW, et al. Postoperative complications associated with reduction malarplasty via intraoral approach: a meta analysis. Ann Plast Surg 2017;78:371-8.

7. Choi BK, Seo JY, Seo HJ, et al. Analysis and guidelines for revisional malarplasty; most common facial skeletal contouring surgery. J Craniofac Surg 2022;33:1674-8.


8. Moss ML, Rankow RM. The role of the functional matrix in mandibular growth. Angle Orthod 1968;38:95-103.

9. Dorfl J. Migration of tendinous insertions. I. Cause and mechanism. J Anat 1980;131(Pt 1): 179-95.
10. Raghuram A, Singh A, Chang DK, et al. Bone grafts, bone substitutes, and orthobiologics: applications in plastic surgery. Semin Plast Surg 2019;33:190-9.



11. Schmidt AH. Autologous bone graft: is it still the gold standard? Injury 2021;52 Suppl 2:S18-22.


12. Zins JE, Whitaker LA. Membranous versus endochondral bone: implications for craniofacial reconstruction. Plast Reconstr Surg 1983;72:778-85.

13. Lee JC, Alford J, Willson T, et al. Improved success rate with corticocancellous block compared to cancellous-only trephine technique in alveolar bone grafting from the iliac crest. Plast Reconstr Surg 2022;150:387e-395e.